A Cancer-Quashing Microbe Emerges from the Deep
A species of marine bacteria shows promise for curing a nasty brain cancer.
Article body copy
Congratulations to Stephanie Stone on winning a Canadian Online Publishing Award for this article.
On August 5, 2017, Amanda Johnson woke up with a headache so consuming that she memorialized her misery. In her datebook entry that day, she sketched a girl with her head crowned in jagged shards of torment, her eyes squeezed shut against the pain. “Headache!!!” she wrote next to the drawing. Downstairs, her parents were making breakfast, but the only thing Johnson could imagine putting into her body was Tylenol. She gulped down two, then made her way to her computer, which was set up on her father’s drawing desk.
Johnson, who was 31 that summer, was living with her parents in Mission Viejo, California, while she finished her second novel—a steampunk saga set in an alternate version of the First World War. She had planned to spend the day editing a chapter, but the daggers behind her eyes persisted, and the screen’s glow seemed to make them sharper. “I tried, but I just couldn’t do it,” she recalls now. “I had to go lie down.” By that afternoon, she was worried enough that she contacted her doctor, who referred her to a neurologist.
Over the next six days, as Johnson waited for the recommended neurologist to return from a vacation, her headache occasionally cleared, but then—invariably—came roaring back. By August 11, the pain had become unbearable, and she had begun to have trouble speaking. Her parents drove her to the emergency room, where an MRI revealed a sprawling tumor that had thrust its fingers into both sides of her brain. Within hours, a neurosurgeon rushed her into the OR to remove as much of the tumor as possible, an invasive procedure that left her in a coma for nearly a week.

Writer Amanda Johnson was diagnosed with a brain tumor just months after this photo was snapped on Christmas Eve 2016. Photo courtesy of Amanda Johnson
While Johnson doesn’t remember much about the immediate aftermath, she slowly began to understand what she was facing. The surgeon had been able to remove enough of the tumor to buy her both relief and time, but much of the cancer remained. And it was one of the worst kinds: glioblastoma—the disease that claimed the lives of both John McCain and Beau Biden. Median survival for patients diagnosed with glioblastoma is just 15 months, making it the most lethal of the brain cancers. Moreover, it can cause a cruel constellation of neurological side effects, including paralysis, speech loss, vision loss, and seizures. But Johnson was ready to fight. And while she didn’t yet know it, she was about to gain a powerful ally. Just over 22 kilometers away, at the University of California Irvine Medical Center, a phase two trial was underway for a new glioblastoma drug derived from an unlikely savior: marine bacteria.
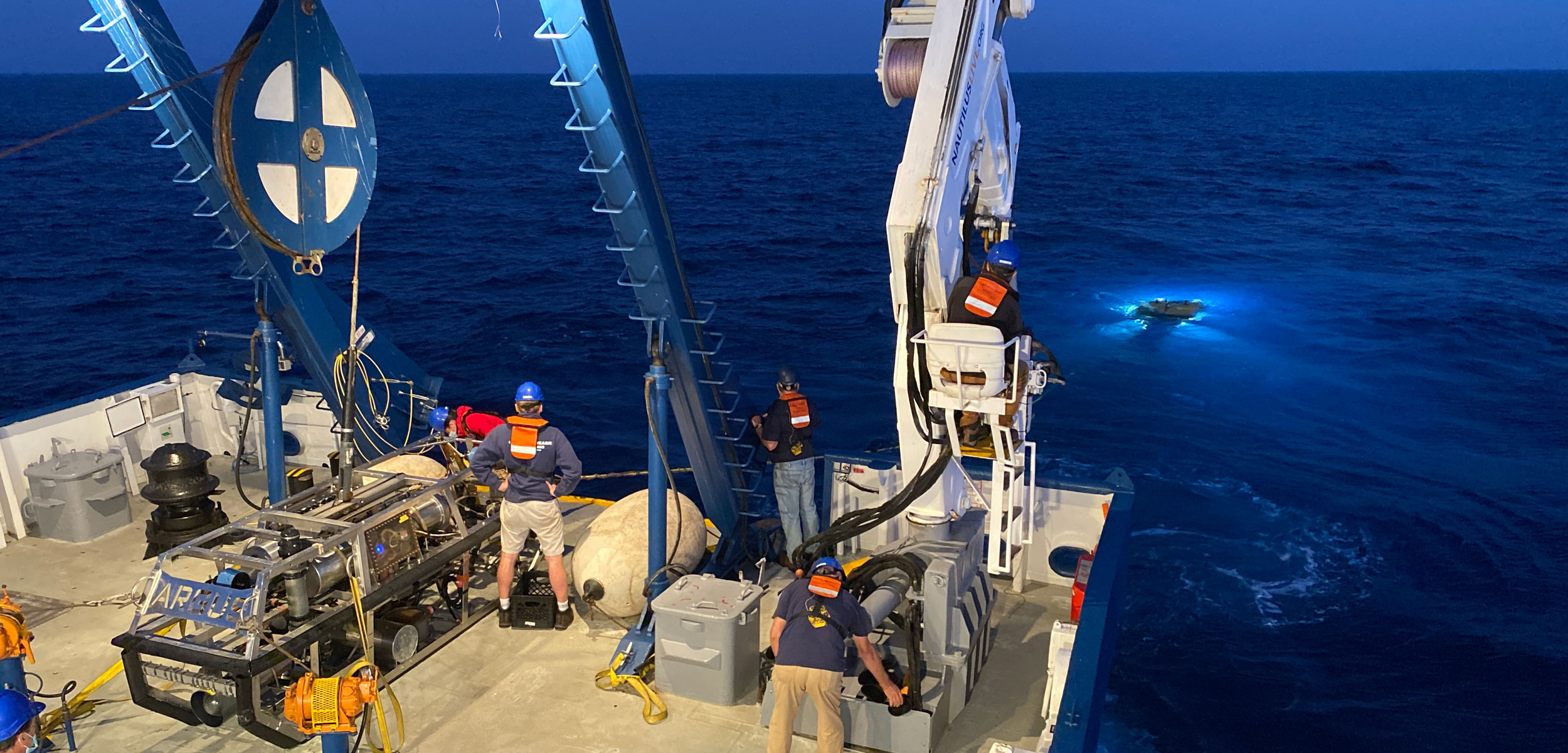
The ROV Hercules descended slowly through dark Pacific waters. A hatchback-sized submersible equipped with video cameras and a suite of sensors and samplers, it was headed for the San Juan Seamount off Southern California’s coast. Hercules pilot Jessica Sandoval maneuvered the sub from the safety of a control room aboard the Nautilus, a research vessel operated by the Ocean Exploration Trust that floated some 560 meters above the seamount’s sunken summit. As she called out course data, tiny translucent bodies drifted up through the submersible’s headlight beams like snowflakes falling in reverse. Occasionally, a larger animal appeared—a pyrosome resembling a glowing cucumber, or a ribbonlike siphonophore with wispy stinging tentacles. But Paul Jensen, a scientist from Scripps Institution of Oceanography at the University of California San Diego, had less flashy things on his mind as he peered over Sandoval’s shoulder on October 30, 2020.
The sediments blanketing the ocean floor and the invertebrates that form its living terrain both contain a wealth of creatures invisible to the naked eye, including marine bacteria. Tiny as they are, these uncharismatic microbes play a critical role in recycling nutrients in the ocean and in feeding other organisms. Many also produce chemicals to defend themselves against predators and microbial pathogens, as well as to communicate and compete with other organisms. Because these compounds can attract, deter, or kill other microbes, some can also benefit people as potent antitumor agents, antibiotics, antivirals, and other drugs. Jensen had discovered dozens of these potentially useful molecules from shallower seas, but he had never before had access to an ROV that could sample at such depths—up to 4,000 meters below the ocean surface. Because deep-sea bacteria face different environmental challenges than their shallower and land-dwelling relatives, the compounds they produce could be unique as well.
As the Hercules cruised slowly along the seamount’s flank, Jensen spotted a bright-yellow octocoral—its soft frame studded with tiny eight-tentacled polyps—and asked Sandoval to collect it. She positioned the ROV’s clawlike collecting arm around the coral’s base.
“Did you ever play that game in the arcade where you have to reach down and grab one of those stuffed animals?” Jensen asked. “You would be really good at that.”
Sandoval scoffed. “Those are totally rigged!” She nabbed the coral and placed it into a white collecting bin.
The idea that nature can yield important treatments for human ailments isn’t new. People have used active compounds from herbal preparations for millennia, and scientists have isolated these compounds for drug development since the early 1800s, when they first synthesized morphine from poppies. Microbes emerged as an important source of new medicines in 1928, when Alexander Fleming discovered penicillin from a mold. Since then, bacteria have proved to be the most valuable microbes for pharmaceutical development. Among the active compounds discovered from microbes to date, more than 60 percent come from bacteria. Nearly three-quarters of those come from a single class of bacteria: the Actinomycetes.
From the 1930s through the 1970s, often regarded as the golden age of antibiotics, scientists discovered a seemingly endless supply of new drugs from soil-dwelling actinomycetes, including tetracycline for pneumonia, erythromycin for ear infections, and most of the other antibiotics we take today. They also isolated the first actinomycete compounds with antitumor properties and developed drugs to treat leukemia, lymphoma, and a number of other cancers.
By the 1980s, however, the supply of novel compounds was drying up. Pharmaceutical company scientists were still scouring the world’s soils for new actinomycetes but were increasingly finding compounds they had already encountered. Meanwhile, bacterial resistance to existing drugs was growing.
Given the clear need for new medicines, a handful of scientists began to question why the pharmaceutical industry had yet to explore marine microbial communities in any meaningful way. In 1988, Jensen, who was then a young laboratory technician, took a job with one of them: William Fenical, a Scripps chemist focused on finding potential medicines in nature.

Paul Jensen, a scientist from Scripps Institution of Oceanography at the University of California San Diego, and his colleagues identified a species of marine bacteria that has yielded big results in the world of cancer treatment. Photo courtesy of Ocean Exploration Trust/NautilusLive
At the time, says Fenical, the consensus among pharmaceutical microbiologists was that actinomycetes lived only on land, and therefore “nothing was important in the oceans.” But Fenical suspected that a sampling bias drove that conclusion, and in June 1989, he and Jensen traveled to the Bahamas to see for themselves, collecting vials of ocean-floor sediment from 15 different locations at depths of up to 33 meters. Back at the lab, it didn’t take long for the two scientists to prove the naysayers wrong. When they cultured their samples, they found 289 separate actinomycete colonies. Some of these bacteria, members of a new genus that they later named Salinispora, had never been documented on land. Moreover, they were most abundant in the deeper samples, suggesting that they hadn’t simply washed into the ocean with terrestrial runoff. And then there was the kicker: Salinispora grew only in salt water.
Working with a team of colleagues, Jensen eventually identified two different species of Salinispora bacteria from the Bahamian samples, both of which produced unique active compounds. One of these species, S. tropica, made a molecule that would change the course of their careers. When Fenical tested it on a line of difficult-to-kill human colon cancer cells, the compound passed with flying colors. He then sent it to labs at the National Cancer Institute to be tested against a panel of 60 different cancer cells. The results were exactly what Jensen and Fenical wanted to see: the compound, which they named salinosporamide A, was especially active against some cancer cell lines, but not others.
“You want that selectivity, because if it kills all cancer cells equally, then it’s probably also going to equally kill noncancerous cells,” Jensen explains. It seemed they had the makings of a viable drug on their hands: a compound that could target a tumor without killing the person it afflicted.
“We saw right away—wow, this looks really good,” says Fenical. “And then we started thinking, What do we do now? How are we going to make sure this gets developed?”
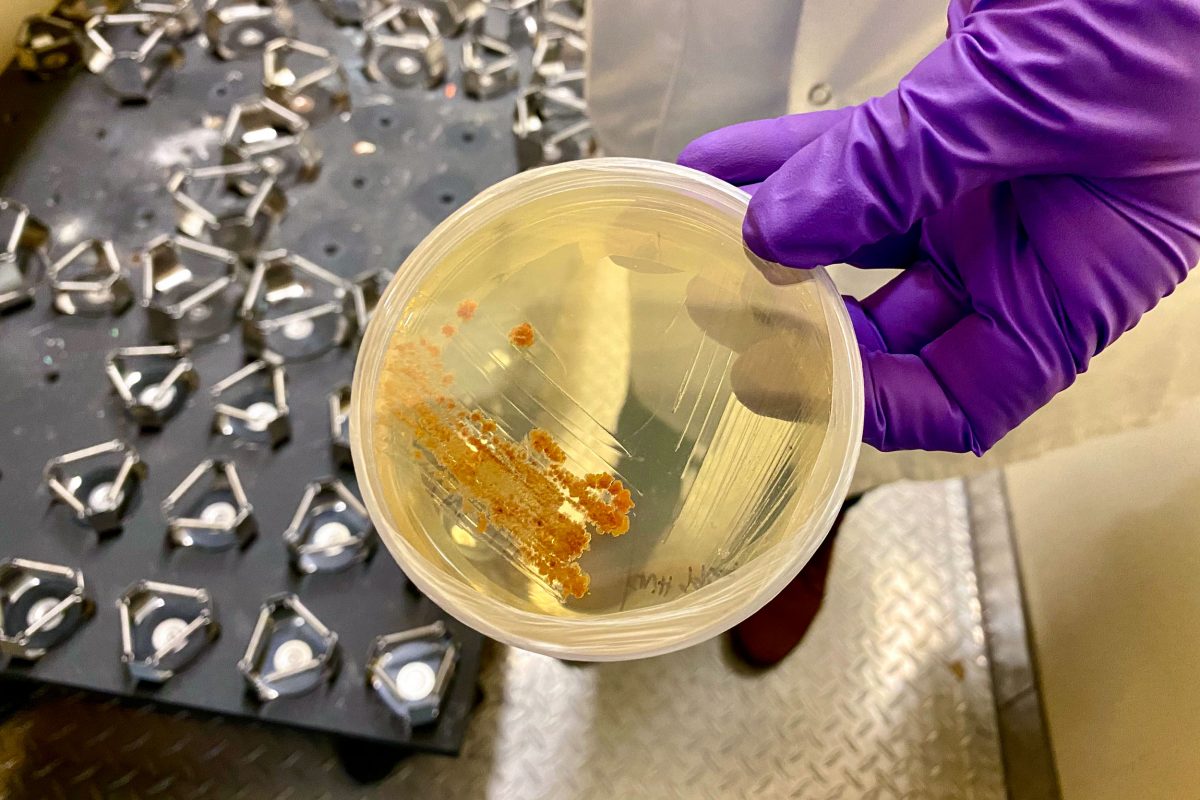
About three months after Jensen disembarked from the Nautilus and delivered two coolers filled with deep-sea invertebrates and sediment samples to his lab, I visited the Scripps campus to meet with Johanna Gutleben, a postdoctoral researcher on his team tasked with DNA extraction. An Austrian native who had just arrived in San Diego in November, Gutleben still hadn’t met Jensen in person because COVID-19 precautions had kept him at home, but she was already well versed in his protocols.
After we donned goggles, gloves, and lab coats, Gutleben led me outside to retrieve some specimens from the neighboring building, a round, sand castle–like construction topped with triangular peaks and surrounded by an empty moat. “There used to be sea lions in there,” she explained, anticipating my question.
The small building once housed laboratories for marine mammal physiology studies. Today, it’s jam-packed with freezers. Gutleben retrieved a plastic bin from one of them and fished through ziplock-encased specimens until she found a sunset-pink bubblegum coral (Paragorgia arborea) and a sponge that looked like a pile of spun sugar, which the scientists hadn’t yet identified. Jensen was particularly interested in the coral, since that species had previously been documented to possess predator-deterring compounds, which are likely produced by bacteria. Gutleben, who did her PhD research on the microbial community associated with marine sponges, was anxious to get her hands on the sponge, since she had never seen anything like it before.
She carried the specimens back in a bucket of ice, then began chopping each sample into bits to break down its cell walls and facilitate the DNA extraction process. As she worked, I thought about how profoundly Jensen’s research methods and tools have changed since his first expedition to the Bahamas. During his early work with Salinispora, he relied exclusively on culturing techniques to isolate strains of bacteria and look for their active compounds. But in 2001, a team of Japanese scientists sequenced the genome of a Streptomyces bacterium and discovered that it had the potential to make many more compounds than they had seen in culturing studies, opening up genomics as a new research avenue for the field. While a genome doesn’t provide scientists with the exact chemical composition of an active compound, it does allow them to predict both the types of molecules a species can produce and the pathways those compounds will act on within a cell, information that can guide their future culturing work.
On the heels of the 2001 study, Jensen and a group of colleagues sequenced the S. tropica genome and found that nearly 10 percent of its DNA—the largest percentage known from any species—was dedicated to producing 17 active compounds, most of which had not been revealed through culturing.
“One of the big limitations of culturing,” Jensen explains, “is that we can isolate bacteria from sediments and grow them in the lab, but obviously the conditions are different, and they may not be interested in producing some of the molecules that they make in the bottom of the ocean.” It stands to reason that if bacteria don’t have to fend off predators, parasites, or competitors, they may not employ their full arsenal of compounds.
Once Jensen and other scientists realized how much more compound potential species like S. tropica held than they had previously known, they began attempting to coax more diverse molecule production out of promising bacterial cultures. Adding toxins and other stressors to the culturing broth or starving the bacteria of certain nutrients sometimes yielded new compounds, as did co-culturing multiple types of microbes—an attempt at mimicking competition in nature.
Today, Jensen, Gutleben, and the other members of their team have even more tools at their disposal to find novel molecules. Instead of isolating a single strain of bacteria and sequencing its genome, they can extract the DNA from entire communities of organisms in a sample—a process called metagenomics—and look for the types of gene clusters that create new compounds. They can also mine all of the molecules in those same samples and look for chemical structures that fit the assembly instructions spelled out in the gene clusters. It’s a complicated matching game, but it’s more comprehensive than testing a single laboratory-grown strain at a time.
Jensen and longtime collaborator Bradley Moore have also begun to leverage the interesting gene clusters they detect during genomic analysis in a new way: using molecular techniques, they insert those genes into a suitable host bacterium, causing it to produce the corresponding compounds during culturing experiments—a process called heterologous gene expression.
Since their initial discovery of salinosporamide A, the Scripps scientists have found more than 100 novel active compounds. Within a couple of hours, they were one step closer to knowing if either the bubblegum coral or the sponge might help them expand that pool of discoveries; Gutleben managed to extract two high-quality vials of genetic material. But when I suggested that she may have just handled a specimen that would lead to the next promising cancer drug, she laughed and offered a reality check. “Yeah, but out of around 1,000 compounds that get detected, only one makes it into clinical trials.”
When the golden age for antibiotic development began to wane in the 1970s, natural-product drug-development programs also withered. Driven by a belief that microbial resources had been overexploited, most pharmaceutical companies gradually shifted their focus to creating synthetic compounds. By the time Fenical and Jensen saw how salinosporamide A performed against the National Cancer Institute cell lines, natural products had fallen so far out of favor that the scientists were unable to convince an established company to develop the compound. Over and over they heard the same thing: no one would take a risk on a natural product without more data, including from animal testing—requirements the scientists couldn’t fulfill in their university labs. Finally, in 1998, they secured an initial round of venture capital funding and launched their own company, Nereus Pharmaceuticals.
Armed with cultures and information from Fenical and Jensen, the scientists at Nereus put salinosporamide A through its preclinical paces. They learned that the compound worked by targeting a cell’s proteasome—a sort of garbage-disposal unit that chews up used and abandoned proteins—and preventing it from functioning properly, eventually clogging and killing the cell. Scientists already recognized this as an important pathway to kill a bone marrow cancer called multiple myeloma, so Nereus focused at first on that disease. By 2007, they were administering salinosporamide A, also called marizomib, to participants in a phase two human trial for multiple myeloma.
Later that year, serendipity joined persistence and temerity as a determiner of the drug’s fate. Daniela Bota, then a fellow in neuro-oncology at Duke University in North Carolina, attended the annual conference for the American Association for Cancer Research, where she listened to Nereus scientists present results from their multiple myeloma trial. Bota was searching for potential glioblastoma treatments, and marizomib intrigued her. While the drug was successfully killing multiple myeloma cells, many of the trial patients reported temporary neurological side effects, including dizziness and speech impairment. To Bota, this suggested that marizomib might be capable of passing through blood vessel walls to access brain tissue directly, something very few cancer drugs can do.

Daniela Bota, a researcher at the University of California, Irvine, who studies glioblastomas and treated Amanda Johnson with medication derived from S. tropica. Photo courtesy of UCI Health
Busy with other projects, Bota didn’t immediately pursue marizomib. But within a few years, her research on glioblastoma stem cells had convinced her to focus on proteasome inhibition as a promising strategy for targeting glioblastoma tumors. While most cancers tend to have lower levels of proteasome activity than regular cells do, this is particularly true for glioblastoma.
“It’s almost like when we build race cars,” Bota explains. “Race cars are missing a lot of the safety and comfort components that you see in a regular car, but they’re made for speed. Evolutionarily, the cancer cells have decided to lose some of those mechanisms just so they can move faster and keep dividing.”
Glioblastoma cells are especially adept at dividing quickly; an untreated tumor doubles in size in just two weeks. But that speed comes at a cost, and Bota hoped to take advantage of the cells’ vulnerability. The problem was that none of the available proteasome inhibitors could cross the blood-brain barrier to target glioblastomas where they bloom. Bota, who by then had started her own lab at the University of California, Irvine, found herself thinking about the Nereus presentation.
She called the company and proposed a joint effort to test marizomib on glioblastoma. Over the next few years, they ran studies on mice and rats, with promising results. But funding was tight, and progress was slow until 2012, when Triphase Accelerator Corporation bought Nereus. The influx of money spurred rapid advances. By 2016, marizomib had progressed to phase two trials for glioblastoma, and pharmaceutical giant Celgene Corporation bought the drug from Triphase. Marizomib’s long and winding journey from seabed to bedside wasn’t quite over, but it seemed to be approaching the finish line.
The day after I watched Gutleben extract DNA from frozen invertebrates, I drove to Mission Viejo to meet with Amanda Johnson. Sitting on a park bench surrounded by pepper trees, she told me about the tumultuous journey that followed her brain cancer diagnosis. When she walked into Daniela Bota’s office for the first time on September 20, 2017, Johnson had never heard of marizomib. She had, however, heard that Bota’s expertise on glioblastoma was unrivaled, and she was prepared to pursue any course of treatment Bota recommended. Her postsurgery MRI had confirmed that a large, comma-shaped tumor still stained her brain. Left unchecked, it would kill her.
By January 2018, Johnson had joined the phase two trial for marizomib. In addition to initial treatment with both radiation and Temodar—a chemotherapy drug that can boost survival by up to six months in glioblastoma patients—she received doses of marizomib on three out of every four Mondays. Johnson responded to the treatment immediately, and each time she got an MRI, she could see that the tumor was shrinking. “I would always be scared when I was going to take another one that it wouldn’t be improving,” she says. “But it did. Every time.”
Marizomib progressed to a phase three trial, and Johnson continued her treatment. Eventually, the tumor shrank to the point that it became unmeasurable. Bota wasn’t sure whether the tiny smudge she could still see on Johnson’s MRI was scar tissue or a few lingering cancer cells. But the scans remained stable, and in January 2021, she and Johnson agreed to suspend treatment. After three years of a grueling regime that left her exhausted and dizzy, Johnson graduated to a much less invasive cycle of care: she would come in every two months for an MRI to make sure the tumor hadn’t returned.

The treatment has paid off for Amanda Johnson; the glioblastoma diagnosed four years ago has not progressed. Photo by Stephanie Stone
While Johnson’s results were remarkable, not all of Bota’s patients in the marizomib trials have done as well. Many reached impressive survival milestones, but older patients were more likely to experience stronger neurological side effects, including confusion and hallucinations. “If you get a drug into the brain, you will see some side effects,” says Bota. “But the question is, Does it prolong people’s lives? Is it a valuable trade-off?”
The phase three trial for marizomib is now in its final months, and Bota expects it will take another year or two to analyze the data before the US Food and Drug Administration can make a final decision on whether to approve the drug. In the meantime, the agency recently authorized a phase one trial to test marizomib as a treatment for diffuse intrinsic pontine glioma, the most common brainstem tumor in children.
The bold decision Fenical and Jensen made to found Nereus has clearly paid off. But it’s not realistic for the scientists to seek venture funding each time they find a promising new compound, says Fenical; as university professors, they must prioritize research and mentoring students. Instead, they’ve tried to convince established pharmaceutical companies to develop the most promising of the antitumor and antibacterial agents they find, without much luck.
Fenical believes that at least 20 of their sidelined molecules could become effective drugs. One, for example, proved to be extremely effective against both anthrax (Bacillus anthracis) and MRSA (methicillin-resistant Staphylococcus aureus), a notorious superbug that has become resistant to many common antibiotics. “The compound was unique from any antibiotic out there,” says Fenical. “And it was beautifully active. So we tried to see if anybody was interested. But we never heard a word from anybody in the pharmaceutical industry, or anybody at all who should have been interested in antibiotics.”
Pharmaceutical companies currently have little financial incentive to develop new antibiotics, because they sell at comparatively low, heavily regulated prices and are prescribed for short periods of time. Yet the need is great: nearly every existing antibiotic has become less effective against at least some bacteria, and public health officials widely recognize antibiotic resistance as one of the greatest threats of our time.
Meanwhile, approved antiviral drugs exist for just 10 of the more than 220 viruses known to infect humans. And as the COVID-19 pandemic has highlighted, there is a glaring need for more antiviral compounds that can be leveraged to treat emerging diseases while vaccine development is underway.
With these challenges in mind, the Scripps scientists have begun compiling a lending library of the molecules they’ve discovered to date, enabling others to easily access and test the compounds. Part of the idea, says Jensen, is to be prepared to act quickly in a crisis. “The next COVID comes along, and people could pull molecules out of these libraries and test them, and boom, you could maybe quickly find a treatment.”
That’s not a hypothetical scenario. Last year, Jensen’s colleague William Gerwick, who manages the Scripps compound library, turned to those collections to search for an antiviral compound that could fight COVID-19. Scientists had learned that the virus that causes the disease uses an enzyme called cathepsin to enter cells and replicate, and they proposed cathepsin inhibitors as a potential source of treatments. Fortunately, Gerwick had encountered cathepsin inhibitors before. In 2009, he and a team of colleagues discovered a cathepsin-targeting compound from a marine cyanobacterium in Panama, which they named gallinamide A. When they tested it on COVID virus cultures last summer, gallinamide A proved to be a potent inhibitor of infection. In May, the National Institutes of Health granted Gerwick approval to begin testing gallinamide A on COVID-infected mice in their labs. If those tests go well, they will proceed to additional animal trials before beginning a phase one human trial.
There is tremendous untapped potential stored in the active compounds that scientists like Jensen, Fenical, and Gerwick have discovered from marine sources over the past three decades—and the need for the solutions they could provide is only growing. Over the next few years, the corals, sponges, and sediment samples currently sitting in Jensen’s freezers will almost certainly yield new compounds that will take their place in the Scripps library. And while the chances may be slim that any one of them will become an approved drug, the possibility that there is another marizomib among them is both real and powerful, provided someone invests in their development.
Not long after I met Amanda Johnson, she emailed me with good news. She had gone in for her first MRI since completing her final marizomib treatment in January, and the scan was completely clean. Four beautiful words were printed across the top of the image: “No evidence for progression.”
We had talked, the week before, about the unlikeliness of it all: that bacteria from the ocean floor would kill her cancer; that two scientists who live just an hour away from her would travel to the Bahamas to find it; that she would happen upon the clinical trial, without looking for it, at just the right moment. As she reflects now on the past four years, Johnson focuses not on the pain, exhaustion, or uncertainty she experienced, but on how lucky she feels. One day soon, she hopes, she might swim in a tropical sea surrounded by tiny, life-giving life forms, and feel indebted to them.